Everything You Need to Know About the Low-FODMAP Diet
Up to 45 million Americans struggle with irritable bowel syndrome, a painful condition that often causes intense bloating, nausea, diarrhea, and other unpleasant symptoms. Even more people suffer from suspected food intolerances that lead to similar syptoms. While there's no single cause or cure for gastrointestinal problems, many people who live with them are prescribed a low-FODMAP diet to bring their symptoms under control. This carefully regimented diet aims to retrain the digestive tract to better tolerate trigger foods and rebuild the gut microbiome from the ground up. So, how exactly is that done?
Our everything-you-need-to-know guide is here to help you better understand who the low-FODMAP diet is designed for, how it works, and how to maintain a whole-food, plant-based diet as you heal your digestive issues. Forks Over Knives spoke with gastroenterologist Will Bulsiewicz, MD, MSCI, who offered his best advice on confidently taking control of your health with the low-FODMAP diet.
In this article you’ll learn:
- What Are FODMAPs?
- What Is the Low-FODMAP Diet?
- Are High-FODMAP Foods Bad For You?
- Who Should and Shouldn’t Go on the Low-FODMAP Diet?
- How Long Should You Be on a Low-FODMAP Diet?
- What Else Might Be Causing Gut Health Issues?
- Can You Be Whole-Food, Plant-Based While on a Low-FODMAP Diet?
- Our Favorite Low-FODMAP Recipes
What Are FODMAPS?
The acronym FODMAP stands for “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols,” which are certain types of short-chain carbohydrates that aren’t easily digested.
Most digestion occurs in the small intestine, where food is broken down, nutrients are absorbed into the bloodstream, and waste is then pushed into the large intestine. But the small intestine has trouble absorbing nutrients from FODMAPs, because the human body doesn’t produce the enzymes needed to break down these specific types of short-chain carbs; instead, it relies on the trillions of microorganisms that live in our large intestine to do this task. When the small intestine encounters FODMAPs it pulls in extra water to move these foods to the large intestine, which can cause bloating and other GI issues.
Once the food reaches the large intestine, gut bacteria begin to ferment it and get it ready for excretion. While this fermentation is a natural and healthy process, the bacteria can produce excessive amounts of gas when encountering difficult-to-break-down FODMAPs, leading to all the unpleasant symptoms associated with IBS.
| Low-FODMAP Foods | High-FODMAP Foods |
|
|
What Is the Low-FODMAP Diet?
While people with healthy gut microbiomes are able to digest FODMAPs without issue, those with sensitive digestive systems have a much harder time. The good news is that your gut can be trained to better tolerate the foods it once struggled with, which is where the low-FODMAP diet comes in.
“The [low-FODMAP] diet is generally reserved for people who are having digestive health problems that include food intolerances,” explains Bulsiewicz. “What that means is that when people consume normal foods in a normal serving size, they have unpleasant symptoms like bloating, abdominal pain, cramping, diarrhea, constipation, and nausea. The [low-FODMAP] diet is an approach that allows them to improve their symptoms and eventually to reintroduce these foods that they have struggled with.”
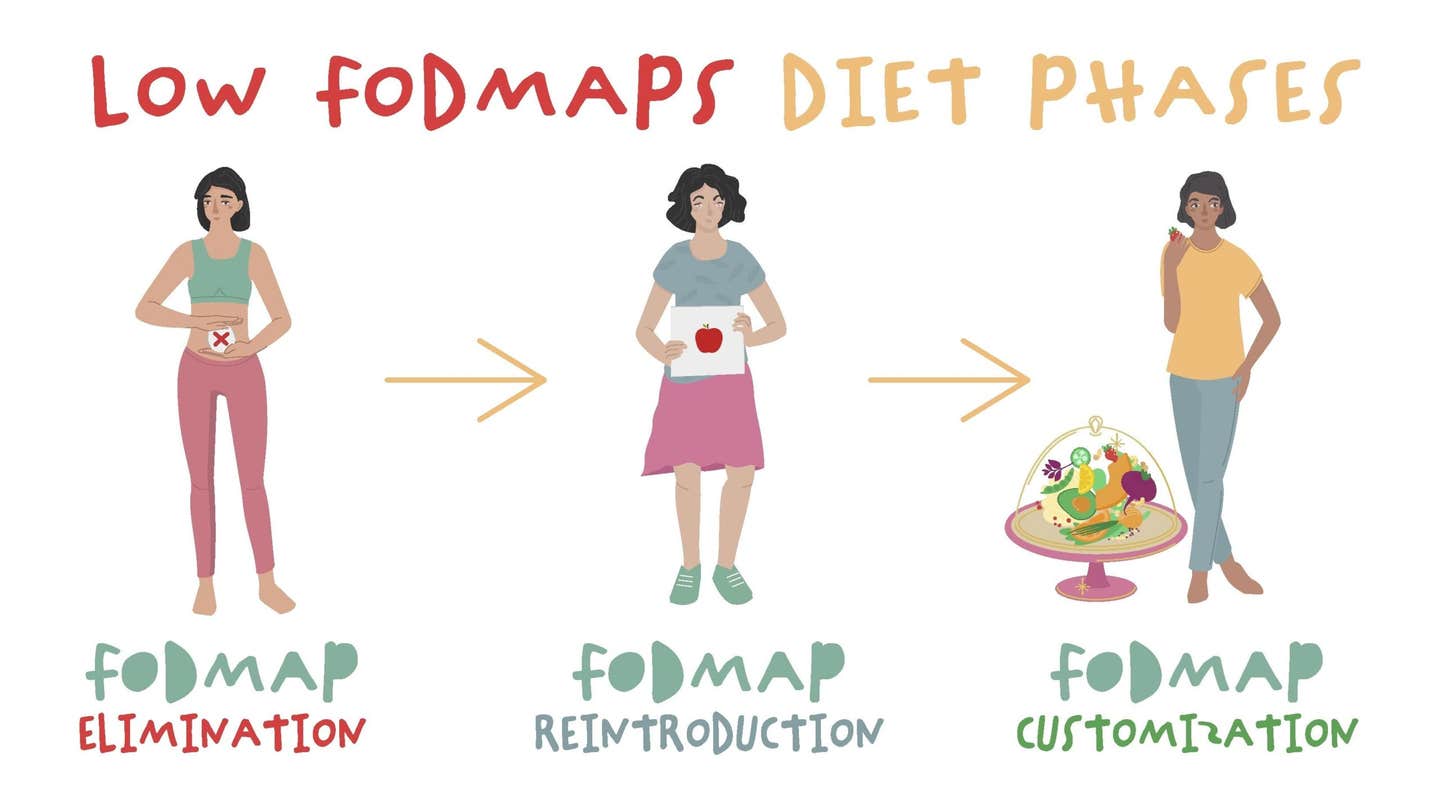
The low-FODMAP diet is typically broken down into three main stages:
- Eliminating high-FODMAP foods from your diet to establish a baseline.
- Reintroducing high-FODMAP foods one at a time so you can determine which are triggering unpleasant symptoms.
- Customizing your diet by figuring out the specific portion sizes of high-FODMAP foods that are tolerable and integrating them back into your normal diet in those portions.
“A properly constructed low-FODMAP approach involves restriction, but it’s just a temporary restriction,” says Bulsiewicz. “Then it's all about reintroduction, which can be quite complicated. Generally, I recommend that people do it with the support of a dietitian or someone who's an expert on the topic.”
Are High-FODMAP Foods Bad for You?
The short answer is no! High-FODMAP foods are not intrinsically bad or dangerous unless you have a specific allergy or condition, such as celiac disease. High-FODMAP foods include fruits, vegetables, and whole grains, which are some of the healthiest foods you can eat.
“The vast majority of FODMAPs are actually prebiotic, meaning that they are good for the gut microbiome,” Bulsiewicz explains. “[By] avoiding high-FODMAP foods, you're depriving yourself of all of the beneficial nutrients that are found in that food, such as polyphenols and phytochemicals and vitamins and minerals. When we categorically remove these foods, it's potentially problematic because not only are we getting into a restrictive dietary pattern where you are more likely to have a nutritional deficiency, but you are negatively affecting the gut microbiome.”
So while it can be tempting to blame your digestive woes on the foods themselves, it’s better to look at the low-FODMAP diet as a technique to slowly make friends with these foods rather than a way to avoid them. Creating a flourishing gut microbiome that can tolerate a wide range of foods is key to fewer digestive problems in the long run and better health throughout your life.
“When you're struggling, it's because the gut microbes are fermenting [FODMAPS] in a way that's inefficient and gas producing,” says Bulsiewicz. “Your gut microbes can be trained to do better.”
Who Should and Shouldn’t Go on a Low-FODMAP Diet?
The low-FODMAP diet is not meant to be a weight-loss technique and should only be used by people struggling with digestive issues related to food intolerances. While weight loss may occur on the diet, Bulsiewicz emphasizes that it’s important to get enough calories and nutrients while on this diet.
“People who have a history of disordered eating should not be doing this, especially not independently,” he recommends. “They should only do it with the approval of someone who’s managing their disordered eating so they can be in a good place before moving forward with it. Also, if a person has a complex medical condition, such as active Crohn’s disease, and they're losing weight, then it’s not the time to do something like this. You have to get your disease under control first before going on a low-FODMAP diet.”
How Long Should You Be on a Low-FODMAP Diet?
The low-FODMAP diet is meant to be temporary, with the goal of resuming more normal eating patterns as soon as possible. Total time spent on the diet will vary from person to person. Typically, the elimination phase lasts two to six weeks and then high-FODMAP foods are slowly reintroduced based on your symptoms and sensitivities. The entire process should only last a few months, says Bulsiewicz.
“Ultimately, we want a diet of abundance,” says Bulsiewicz. “The most important rule for gut health is to eat a wide variety of plants. The advantage of a properly constructed FODMAP approach is that it allows you to, number one, feel better. Number two, understand what the source of your problem is. Then number three, to actually have a strategy to bring that food back on board and tolerate it.”
Bulsiewicz says that you'll know the low-FODMAP diet has worked once you're able to enjoy a wide variety of foods free of unpleasant symptoms. Remember, the idea of going on the low-FODMAP diet isn’t to eliminate large categories of food: It’s to slowly retrain your gut microbiome to tolerate the foods that typically trigger it.
“Ease into it and give your body a chance to catch up and adapt to what you're doing,” Bulsiewicz recommends. “It’s similar to exercise. If you haven’t worked out in a while, you wouldn’t pick up the heaviest weight in the gym. You’d start small and work your way up from there. It’s the same with high-FODMAP foods. As with anything, you’ll get better the more you practice.”
What Else Might Be Causing Gut Health Issues?
There are myriad other reasons for digestive problems besides FODMAP sensitivities. As you work on retraining your gut, it’s likely your physician will also recommend lifestyle changes to help bolster the impact of your dietary changes. Bulsiewicz says there are many aspects of our modern lives that lead to gut issues.
“It's the lack of sleep, it’s the electronics in the evening before you go to bed, it’s the absence of exercise, it’s the medications, and it’s the large amount of processed foods present in our diet,” he says. “These are all disruptive to the balanced community of microorganisms in our gut.”
Stress can also play a significant role in chronic gut health problems. A 2020 review published in Current Opinion in Behavioral Sciences indicates that the relationship between our mental health, gut microbiome, and dietary choices is deeply interconnected. Depression, anxiety, and other psychological conditions can influence the reactivity of gut bacteria and cause flare-ups of digestive issues. When beginning the low-FODMAP diet, be sure to talk with your doctor about how mental health may be playing a role in your intestinal discomfort.
Can You Eat Whole-Food, Plant-Based While on a Low-FODMAP Diet?
The low-FODMAP diet was created with omnivores in mind, which means it can often be more restrictive for people who follow a whole-food, plant-based diet since meat and dairy are already off the table. Bulsiewicz shared some thoughts on how to get enough calories and nutrients as a vegan who’s traversing the low-FODMAP path.
“I think it's important to include all of the major [plant-based] food groups,” he says. Don't eliminate an entire group of food. Instead, opt for low-FODMAP options within that groups. “For example, people may often have issues with whole grains, and those issues are usually specific to wheat, barley, and rye. You can opt for a low-FODMAP option like quinoa.”
While we always recommend going directly to your doctor for health care advice, you can check out this full list of FODMAP foods to get a general idea of what you’ll need to eliminate if you’re exploring a low-FODMAP diet. Bulsiewicz also offers an online class in FODMAP intolerance that includes techniques on reintroduction, healthy recipes, and handy kitchen tricks.
“Be patient, because it takes time,” Bulsiewicz recommends. “It’s not meant to be a quick fix. It's meant to be about your long-term health and allowing you to have a diet that is sustainable and enjoyable.”
Our Favorite Low-FODMAP Recipes
High-FODMAP foods such as beans, wheat, lentils, and fibrous veggies are some of the healthiest foods on the planet, and diets rich in these foods have been linked to lower rates of heart disease, certain cancers, and Type 2 diabetes. However, should you need to temporarily cut back on these foods to retrain your gut, here are some healthy WFPB recipes you can enjoy on a low-FODMAP diet:
About the Author

About the Author
Megan Edwards
Join our mailing list
Get free recipes and the latest info on living a happy, healthy plant-based lifestyle.
By providing your email address, you consent to receive newsletter emails from Forks Over Knives. We value your privacy and will keep your email address safe. You may unsubscribe from our emails at any time.
